Blog
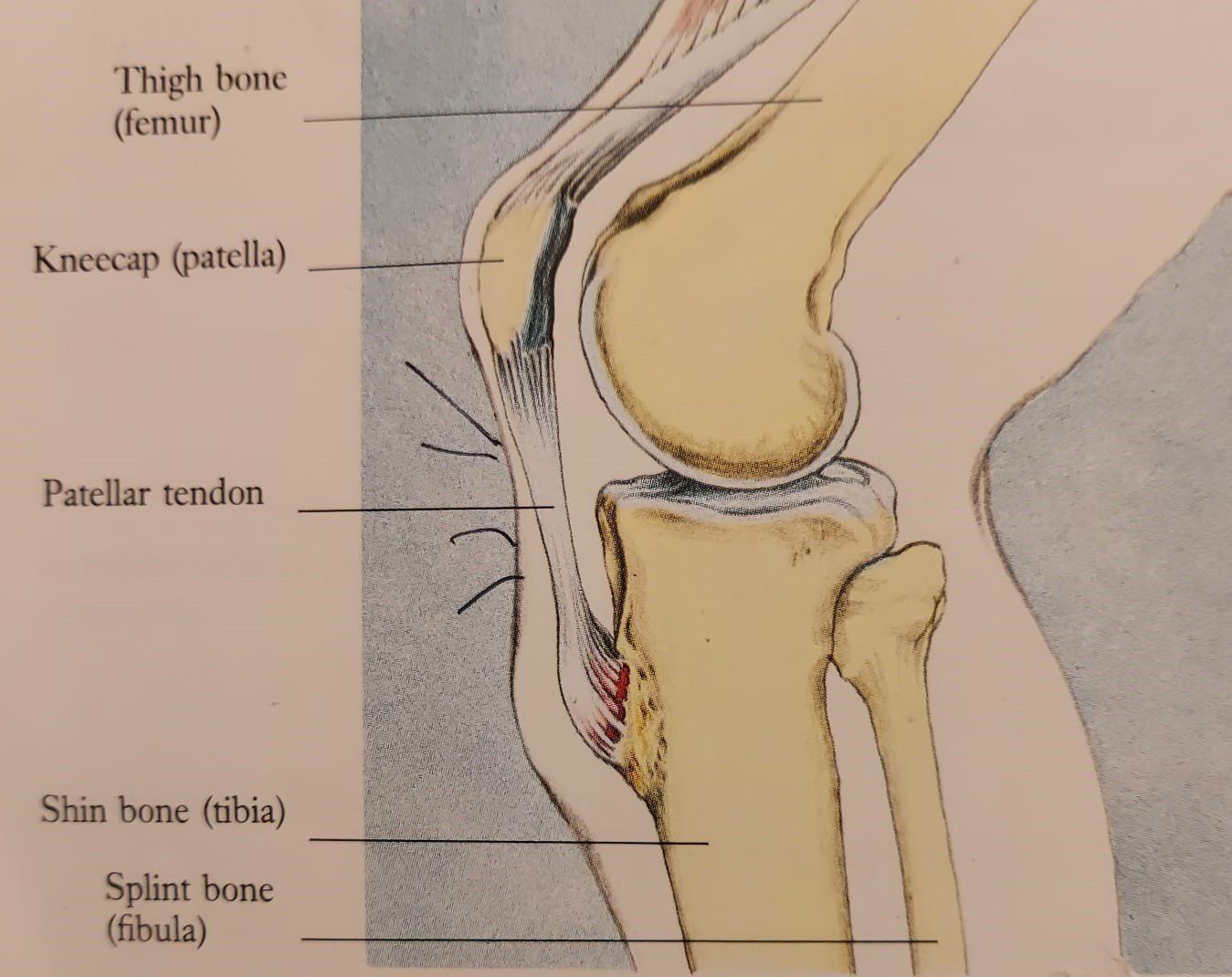
We see many young aspiring athletes and dance performers between the ages of 11 to 16 with this condition. Children are particularly prone during their teenage years of growth as their bone tissue is still developing. Cause It’s caused by an overload or over use on the quadriceps (muscles at the front of the upper thigh) that function to flex the hip and extend the knee. The condition is also enhanced by the fact that young bones are still in growth, with the bone growing faster than muscle, thus the muscle becomes tight creating a pull on the tibial tuberosity (a protruding piece of bone) at the upper part of the tibia (shin bone). Pathology The condition manifests at the insertion of the patella tendon (the distal tendon part of the quadriceps) that inserts into the tuberosity in the upper tibia. Creating an inflammatory reaction in the patella tendon insertion (tenoperiostitis), the periosteum (bones skin) and tibial tuberosity itself. The patient often displaying symptoms of patella tendinitis at the same time. Anatomy and Physiology The make-up of this muscle / bone connection or attachment of a muscle to a bone involves a gradual transition from the elastic muscle to tendon to cartilage to bone. This gives the reasoning why these injuries take so long to heal as the bone / tendon junctions are poorly supplied with blood because the fibrocartilage creates a barrier, making the injury often chronic. Factors It can be attributed to the patient participating in too much sporting activity, increased demand over muscle and insertion capability, not reducing or stopping sport when initial symptoms occur, not having enough rest periods between activities. As the constant strain takes place on the muscle and its insertion, it results in micro muscle fibre ruptures and minor bleeding causing traction, irritation, and inflammation of the soft tissue. Common signs symptoms Local pain around and on the tibial tuberosity, especially on touch. Local swelling and a distinctive prominence around tibial tuberosity. It may affect both knees. The pain is frequently made worse by high impact and deceleration activities such as running, jumping, and cutting, quadricep stretching and contraction. Kicking and squats also play a major part in irritating the tissue. Stages of Injury The degree of injury is evident when the young performer experiences constant pain. In severe cases they cannot run or compete in sport, training session or activities without localised discomfort or pain. There’s pain on resisted quadriceps contraction or full quadriceps stretching. The patient is usually left with a painless growth of bone at the tibial tuberosity once healed that lasts for life. In mild cases, there’s local tenderness, or soreness after activity which quickly disappears. There are some key aspects in the identification and diagnosis along with treatment management, but the secret is to have it diagnosed and treated early.

Understanding Our Blood Pressure High blood pressure (Hypertension) is probably the most seen condition in society today. That said in many cases our lifestyle choices can have a profound effect on its levels and function. Our daily habits like consuming too much salt, smoking, alcohol consumption, drinking caffeinated beverages or carbonated drinks, lack of exercise, not controlling our body weight, to name a few add to the cause of the condition. Its effects can have a major impact on the workload of our cardio vascular system, as arteries have to work harder and their delicate membranes become damaged, bad cholesterol forms plaques and micro tears, the arteries become narrower and although they are usually stretchy, lose their elasticity and become stiff or narrow increasing Blood Pressure. What is Blood Pressure? Blood pressure is the pressure of blood in your arteries, the vessels that carry blood from your heart to your brain and the rest of your body. We need a certain amount of pressure to get the blood moving around our body. Our blood pressure naturally goes up and down throughout the day and night, and its normal for it to go up while moving about High Blood Pressure is when our overall blood pressure is consistently high even at rest and is usually established by an appointment with your GP. Low Blood Pressure (Hypotension) is when your blood pressure is below 90/60mmHg. This does not necessarily mean that there is a problem. How is Blood pressure measured? Blood pressure is measured in millimetres of mercury, mmHg, using a sphygmomanometer (pronounced svig-mo-man-ometer) This is usually a digital electronic monitor, which is connected to an inflatable cuff that is wrapped around your upper arm. When you have your blood pressure measured, the reading is written as two numbers. The first is when the pressure is at its highest, Systolic pressure and the second is at its lowest diastolic pressure. What are Systolic and Diastolic? • Systolic Pressure – This is the highest level of your blood pressure and happens when your heart beats and contracts to pump blood through your arteries. • Diastolic Pressure – This is the lowest level of your blood pressure and happens when your heart relaxes between beats. High Blood pressure is serious. If we ignore it, it can lead to heart and circulatory diseases like heart attack or stroke. If your systolic blood pressure is more than 129 mm/Hg or your diastolic blood pressure is higher than 79mm/Hg all of the time, you will have high blood pressure. This will increase the workload on your cardiovascular system and can lead to serious health problems. If the arteries that carry blood to your heart get damaged and clogged, it can lead to a heart attack. If this happens to the arteries that carry blood to your brain it can lead to a stroke. What is a healthy or normal blood pressure? Your blood pressure should be under 140/90 mmHg. Low • Systolic: lower than 90 mmHg • Diastolic: lower than 60 mmHg Normal • Systolic: lower than 140 mmHg • Diastolic: lower than 90 mmHg Possible hypertension • Systolic: between 140 and 180 mmHg • Diastolic: between 90 and 110 mmHg Severe hypertension • Systolic: higher than 180 mmHg • Diastolic: higher than 110 mmHg What causes high blood pressure? There isn’t always an explanation for the cause, in a small number of people, the cause can be identified but most people develop symptoms because of their diet, lifestyle or medical condition. Sometimes it runs in families and can also worsen with age, however you may still be able to improve it by changing your diet and being active. Doctors sometimes call this secondary hypertension. Causes of secondary hypertension include kidney disease, diabetes, and some medicines, such as oral contraceptives and some over the counter and herbal medicines If you are concerned that any medicine or remedy might affect your blood pressure, consult with your doctor. Symptoms of High blood pressure High blood pressure rarely has noticeable symptoms which is why it is so important to get your blood pressure checked. However, some people can experience blurred vision, nosebleeds, shortness of breath, chest pain, dizziness, and headaches. Over time it can lead to heart conditions, stroke, kidney disease… How to prevent and improve your High Blood Pressure Unfortunately, there is no magic cure for High Blood Pressure but changing your lifestyle can significantly lower the risk. Working with your GP is important not only to establish your blood pressure levels and monitor but also, they may prescribe medicine to help control. But without doubt making healthy lifestyle changes can help. For example, losing weight and exercising for 30 minutes a day, (always seek medical advice before starting any exercise or weight loss plan), eating a healthy balanced diet to include a high potassium content and low salt intake which will reduce the tension in the blood vessels, fish containing omega-3 fatty acids twice a week, as omega-3 has been proven to reduce blood pressure, foods with magnesium and fibre to reduce the risk of heart disease, and reduce alcohol, smoking and processed foods. Info-Physio Gordon Ellis
Multiple sclerosis is one of the commonest central nervous system diseases. In the UK alone there are around 100,000 people recorded as having the condition, mostly diagnosed between the ages 20 and 40. It's well reported that in the Dales in County Durham there is a higher percentage than many other locations in the UK. The condition is caused by damage to the myelin sheath, a fatty material that insulates nerves. Imagine it being like the protective covering around the wires of an electric cable. The myelin protects the nerve and helps it transmit and receive its information. With the loss of myelin (demyelination) its accompanied by a disruption in the ability of the nerves to conduct electrical impulses to and from the brain, producing the varying symptoms we know as MS. The sites where myelin is lost are called plaques or lesions and appear as hardened scar areas. These scars appear at different times and in different areas of the brain and spinal cord. The term multiple sclerosis meaning ‘many scars’. The symptoms vary widely and may include weak limbs, tingling, blurred vision, unsteadiness and fatigue, immobility and spasticity in limbs. For some its characterised by periods of relapse and remission while, for others, it has a progressive pattern. But for everyone with MS, it makes life very unpredictable. Over many years I've studied and worked with MS patients, the range of its effect varying considerably from individual to individual. On speaking to many diagnosed with the condition, a considerable amount feel once diagnosed little is done to help when they return home. There is life after MS and many things that can be done. Having ran a successful MS group I would like to suggest the following. • Become more educated on your condition, what it is, what causes it, how it can be helped by "yourself" and others. • Don't deal with it alone, it can be an isolating, lonely disease. Make an effort to get out and meet others in a similar situation. You may find they have information that can help your condition and your quality of life. • I understand how heavy that set of armour can be somedays, but find anchors to help you motivate yourself. • Make sure your treated and given rehabilitation by or under the guidance of a professionally qualified person with a specialism in this condition. • Have a specialist devise you a home exercise program, that can be administered by yourself or others. Sometimes the up evil of travelling to and from hospitals with long spaces in between can cause more problems. • For the carers, you to struggle with the impact MS. Make time to look after yourself, so you can be strong enough to deal with the person your caring for. Ideas to try • Light massage: Reduces stiffness and oedema, increases flexibility and mobility. It can also alleviate fatigue and pain, whilst improving mood. • Active and passive range of movement to all joints: This helps to work the joints and keep them healthy, reducing stiffness and spasticity. • Active and passive muscle stretching: This helps to prevent and control muscle contracture and spasm, which limits the effectiveness and muscle function. • Seated and standing strengthening of muscles around joints: This will improve your posture, help you to do more, gain better balance and improve your confidence when out and about or around the home. • Manually dexterity exercise: Can help you with picking up a cup or writing. • Temperature: MS is sensitive to temperature, especially heat. • Breathing exercises: So important, If you think everything that happens in our lives physically and emotionally effect out breathing, so breath work can effect your emotion and physical activity. • Relaxation and meditation: With all trauma there comes anxiety, tension and stress which may lead to depression. Relaxation with meditation not only helps with the above, it will help to calm and control your condition along with breathing techniques. • Consider alternative medicines and alternative therapies through discussion with our GP. • Standing and walking to improve your bone strength. • Nutrition: Intake of the correct food and fluids to help your condition and immune system. • Incontinence and pelvic floor problems can become problem: By doing muscle training exercise you can control this. • Isolation, loneliness: keep in touch with friends, family and join groups. Physiotherapy can help to assess physical difficulties, improve movement, teach you exercises to maintain independence. Working holistically as part of a multidisciplinary team, whether your a GP, physiotherapist, counsellor, nurse, speech therapist, masseuse, complimentary therapist, dietician etc.... helping the MS patient and their carer receive the best support they can.
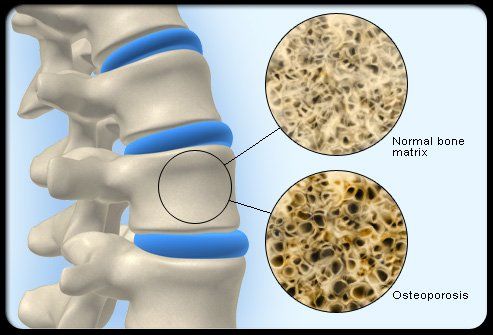
In the UK alone Osteoporosis affects over 3 million people. With more than half a million people each year receiving treatment for fractures as a direct result of the condition. There's not a week goes by in my clinic where I don't see someone who suffers with some form of Osteoporosis, this week alone I had two patients with vertebrae collapses in the spine caused by it. Lowering of our bone density is a normal part of ageing, however the condition makes bone loss take place much faster, creating a weakness to our bones, with the bones becoming susceptible to fracture. In most cases it develops slowly over several years, often being identified after a fracture has been found. When a women goes through Menapause her hormones change, due to this her oestrogen levels fall, therefore increasing the risk of Osteoporosis making women more at risk than men, particularly if the menopause begins early or their ovaries have been removed. However it does affect men, younger women and children. The word broken down Osteo (bone) porosis (porus) meaning the bones density becoming less compact. Homeostasis is our bodies internal mechanism working in balance, constantly connecting and communicating its systems with each other, always constantly changing. Part of this physiological process takes place in our skeletal system where Osteoblasts (bone builders) work in synergy with Osteoclasts (bone clearers) constantly restructuring and creating new bone, until something occurs to disturb the balance and our bone builders reduce. Think of the scenario whereby you put food on a plate for someone to eat, through their craving they eat all the food.. everyones happy and this process continues. Then you stop providing the food, but the person still wants the same amount and starts to eat into the plate itself.. You may have heard the word Osteopenia, this is the stage of bone loss before osteoporosis. There are many other factors that can increase the risk of developing osteoporosis, these include; • Heavy or constant drinking of alcohol and smoking • Not exercising regularly • Family history, particularly a hip fracture in a parent • Long-term use of certain medicines that can affect bone strength or hormone levels, such as anti-oestrogen tablets that many women take after breast cancer. • Taking high-dose steroid tablets for more than 3 months • Other medical conditions – such as inflammatory conditions, hormone-related conditions, or malabsorption problems • Having or having had an eating disorder such as anorexia or bulimia • Having a low body mass index (BMI) If you're worried visit your GP and if they suspect Osteoporosis or Osteopenia they can work out your future risk of breaking a bone using an online programme, such as FRAX or Q-Fracture. They might also send you for a bone density scan (DEXA scan) to measure your bone strength. Its calculated as a standard deviation (SD) and is called a T score. • A T score of -1.0 or obove is normal bone density. • A T score between -1.0 and -2.5 shows low bone density, and is defined as osteopenia. • A T score of -2.5 or below shows bone loss and is defined as osteoporosis. As a treatment your doctor can prescribe bone strengthening treatment and medications, this will depend on your bone density results. Treatment for osteoporosis is based around what i call the 4 P's precautions - prevent - preserve - promote: Where possible you can take precautions through life style choices to lower the risk of the condition taking place. When your diagnosed you can create a treatment plan to live a life that prevents your condition deteriorating and preserves the bone condition you have, to promote bone stability and strength by adjusting what happens to your bodies internal environment and reducing risk from factors of your external environment. Whilst treating and preventing broken bones, and taking medicine to strengthen your bones, through the NHS and your GP. If you're at risk of developing Osteoporosis, or you've been diagnosed, you can take steps to help keep your bones healthy such as; • Making lifestyle changes – such as giving up smoking and reducing your alcohol consumption • Healthy eating, including foods rich in calcium and vitamin D • Taking a daily supplement containing vitamin D and C. • Taking regular exercise little and often, to keep your bones as strong as possible • Avoid high impact activity, and focus on regular low impact and weight bearing activity. • Strengthening your muscles at the major joints. • Educate yourself and read more about prevention and treatment • Speak to your GP • Contact professional organisation such as the NHS and the Royal Osteoporosis Society. • You may find it helpful to talk to a trained counsellor. Physiotherapy can play a major part in giving advice, treatment and rehabilitation for the condition and I would recommend both sufferers and medical practitioners to look up Wolff's Law related to Osteoporosis, I use the theory when treating the condition and it works very effectively. To read more about prevention, treatment, Wolff's Law, physiotherapy rehabilitation exercises and classes, visit my website or our Facebook page. Like all other articles i will be writing in the Gazette you'll find a more detailed account of the conditions I cover there. For anyone who would like to send questions into the paper on this subject, please feel free. For more information or further advice, guidance or treatment related to this topic please contact Gordon on: Tel: 07985 610434 / 07368 220733 Website: www.info-physio.com Facebook info physio / Gordon Ellis Email: physio-gellis@hotmail.com
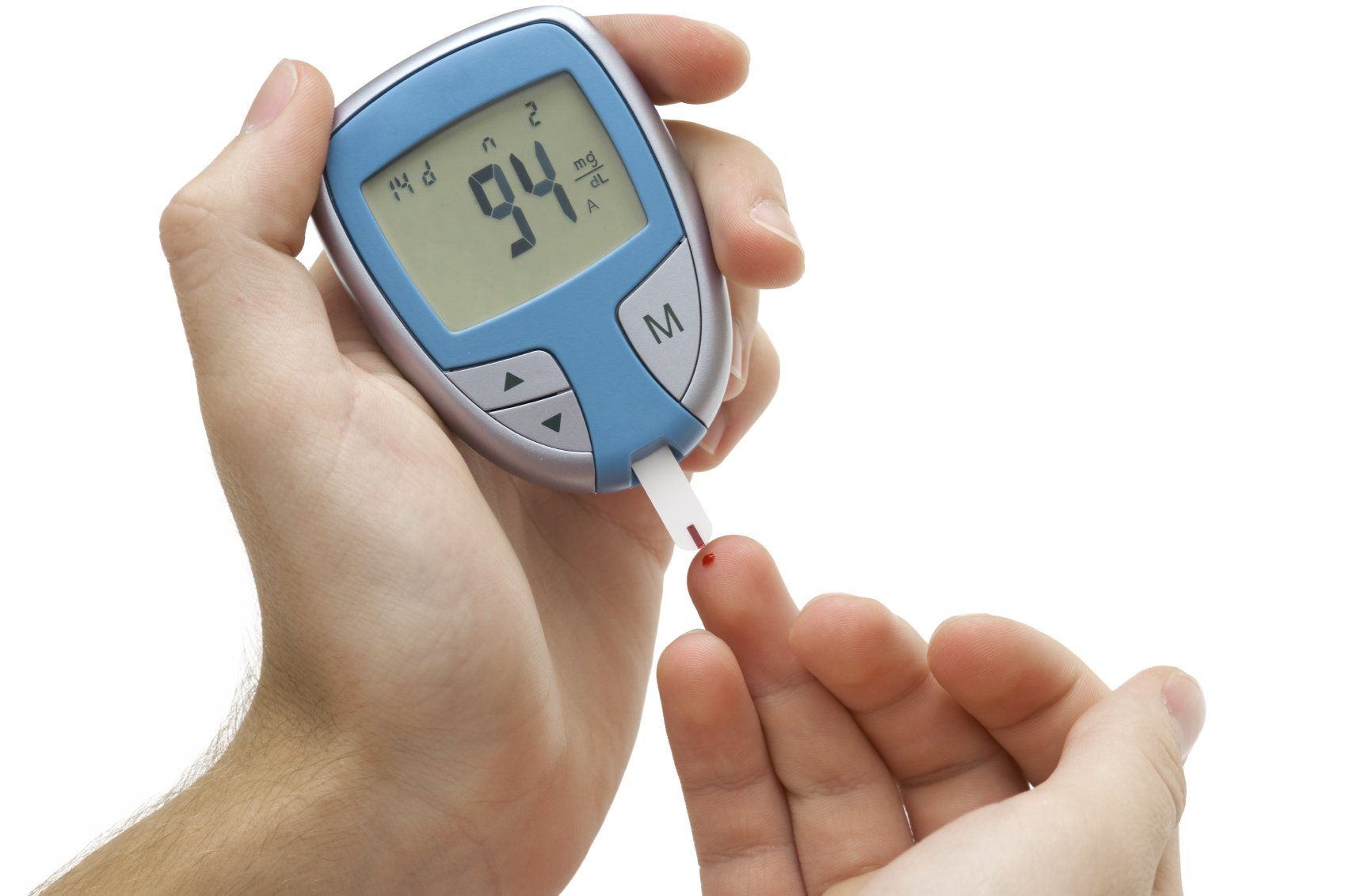
For many of us Diabetes is something we hear talked about, but never totally comprehend the seriousness of the condition. In its simplest form, its a serious lifelong condition where a person's blood glucose (sugar) level is too high, falling into two main categories; Type 1: Where the body's immune system attacks and destroys the cells that produce insulin. Type 2: Where the body doesn't produce enough insulin, or the body's cells don't react to insulin. In both cases, if glucose is unable to get into our cells effectively, it creates too much glucose in our blood, causing complications and problems. Glucose comes from the carbohydrates we eat and drink, helping to give our body energy. It works alongside a hormone called insulin that's made by our pancreas, the insulin allowing the glucose to enter our cells from our blood. Diabetes can have the following symptoms, but not in all cases, in fact type 1 on occasions can be mistaken for a virus, so this is far from an exhausted list and with type 1 and 2 the symptoms can differ. In all cases it's better to check out the specific symptoms related to your condition. You may experience feeling hot sweaty, very thirsty, very tired, mood swings, blurred vision, peeing a lot especially at night, weight and muscle loss, itching around the penis or vagina with symptoms of thrush, cuts that seem to heal slowly. I can't stress enough If you are in any doubt or worry, seek help from a professional person by going to see your GP as soon as possible for advice. Once diagnosed you'll need treatment. In the case of Type 1 it will be insulin delivered daily by injections or pump therapy. In the case of Type 2 it will be finding the right medication through your GP, as some may have side effects. Then learning how to measure and control your levels by interventions yourself. Have regular checks, learn to carb count and monitor your blood glucose levels so that they stay balanced. It's important also to have a balanced healthily eating regime, taking regular light exercise. You may have heard the terms Hyperglycaemia and Hypoglycaemia. These describe when the blood sugar level is high (Hyperglycaemia) and when the blood sugar level is low (Hypoglycaemia) It's difficult to write about diabetes when there's so much to cover, such as pregnancy, eye screening etc.. My advice would be to speak with your GP, read credible sources of literature such as the NHS and Diabetes association, join support groups, carry some form of medical ID with you and attend a course on managing your diabetes. In all aspects of diabetes, modern technology has improved, improving life expectancy. However how you deal with your 360 degree personal heath investment will contribute a lot more. Life doesn't end just because of diabetes. This statement doesn't just apply to the patient, it's also for the carer who devotes a large amount of time supporting and helping. You can still do everything you did before, its more about life style choices, education and time management that reduce or increase its impact. The most important message to leave the reader with... Remember you control your diabetes, don't allow it to control you, and with all conditions the quicker it's diagnosed the more effective the treatment..








